Happy families
Date published: 05 January 2016
FORMER Chronicle reporter Janice Barker’s new grandson Felix is one in more than five million IVF babies born in the past 37 years.
Felix wouldn't be here without the pioneering work of two men whose research put Oldham, and Louise Brown, the world's first test tube baby, on front pages in 1978 - a story in which the Chronicle - and Janice herself - led the world’s media. Here Janice takes up the story...
MILLIONS of parents now have the joy of their own child only because of the “magnificent obsession” of consultant gynaecologist Patrick Steptoe, and the research of Dr Robert Edwards.
The pair fought for 12 years to perfect the technique before Louise was delivered at what was then Oldham and District General Hospital on July 25, 1978.
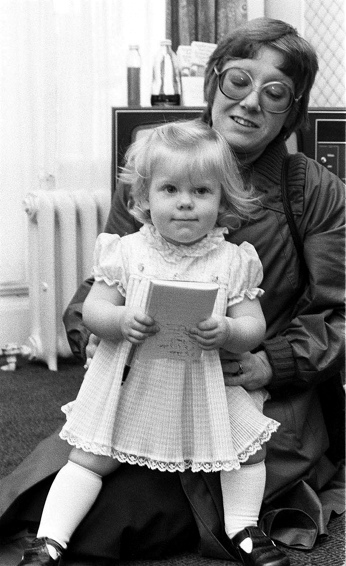
Felix is also an IVF baby, born to my daughter Jennifer a few weeks ago.
Jenny and husband Lewis already have a child, our grandson Rueben, now four. But just like Lesley Brown, Louise’s mother, Jenny found she had damaged fallopian tubes which meant she couldn’t conceive a second child naturally after an ectopic pregnancy in 2013.
Back in 1977, Lesley Brown and her husband John had tried for nine years to have a child and an operation to unblock her fallopian tubes was unsuccessful. Luckily, Lesley’s GP happened to have heard of the early work by Steptoe and Edwards.
They had shocked the scientific world and put Oldham in the headlines in 1969 when they confirmed they had fertilised a woman’s egg outside the body. Two years later they revealed they had repeated the experiment and implanted a fertilised human egg in the womb though it had died.
Lesley’s GP wrote to suggest her for treatment. In the book “Our Miracle Called Louise”, written by Lesley and John and published in 1979, Lesley said: “It was a million-to-one chance.”
Mr Steptoe took her on and Lesley joined a list of over 400 women who had pinned all their hopes of a child on a unproven technique being developed at Oldham and District General and a small cottage hospital, Dr Kershaw’s in Royton.
But time was running out. The first woman to carry an IVF baby to early pregnancy, Marlene Platt in 1975, had lost the child to an ectopic pregnancy. Another woman’s pregnancy had also failed, and Mr Steptoe was due to retire in June 1978, was on a shoestring budget, and soon Dr Kershaw’s would become unavailable.
Lesley had been treated at Dr Kershaw’s in November 1977 and as Dr Edwards watched through a microscope, fertilisation took place and the potential baby began to grow until the developing baby was a cluster of cells large enough to place into Lesley’s womb on November 12.
Then two miracles happened: John won £800 on the pools, to pay for their travels from home in Bristol to Oldham. The second was that just before Christmas 1977, Lesley was told by Dr Edwards that she was pregnant.
Though Mr Steptoe reassured Lesley she wasn’t the only woman being treated, what she didn’t know was that as the months progressed, she was the first woman to successfully carry the child towards full term.
The Chronicle’s news editor at the time was Peter O’Reilly, who had been interviewing the Oldham Area Health Authority’s administrator, Edwin Warren, when the health official dropped into the conversation that the baby would be born at the Oldham hospital in the Marron maternity unit. The news was on the Chronicle’s front page the next day and we continued with exclusive after exclusive.
The bombshell sent shockwaves around the world, and teams of foreign journalists and film crews descended on the town and hospital - known then as Boundary Park, now rebuilt as the Royal Oldham.
The authorities were completely unprepared for the overwhelming coverage and mothers and babies leaving hospital, visitors to the maternity wards and hospital staff were all grilled about what was happening inside.
But with good contacts and using many sources who had been keeping the Chronicle abreast of what was happening, the team of four — Peter, his deputy Mike Attenborough, myself and health correspondent Susan Pape — were able to continue producing world exclusives - including how Mr Steptoe was preparing for a Caesarian delivery on July 26. We were only 13 minutes out when Louise was delivered at 11.47pm on the 25th, weighing 5lb 12oz.
The whole birth was filmed by a crew from the Government information service, COI, to show that Lesley was the mother, the baby was born healthy and crying lustily — there had to be no doubt that it was Lesley’s baby and she could not have conceived her naturally.
Louise was the first and only baby born by IVF at Oldham hospitals. The first boy, Alistair McDonald followed six months later in Glasgow. Mr Steptoe raced up there but was delayed by snow and missed the birth.
My daughter’s birth of Felix was much more low key, but because she already had a son, she and Lewis had to turn to a private clinic and pay for treatment. This is one of the major changes since 1978 — when Bourn Hall in Cambridgeshire was opened by Mr Steptoe and Dr Edwards in 1980 it was the UK’s first and only private IVF clinic.
By 2013 the Human Fertilisation and Embryology Authority reported there were 78 clinics in the UK performing IVF, and the Government also suggested infertile couples with no children from a previous relationship could be offered up to three cycles of IVF free on the NHS.
Private treatment comes at a cost, and Jenny and Lewis had to save hard. They paid a four figure sum and had two implantations, one unsuccessful. The second resulted in Felix on October 9.
Jenny said: “I didn’t find the drugs regime and having to do my own injections gruelling as some people do, but I’m not naturally squeamish.
“After the egg recovery we had nine eggs, and you get a phone call from the clinic to say how many have made the grade. It is like they are looking after them in a little nursery! In total we had five fertilised eggs. They are grown to a certain stage, called blastocyst, which increases their chances of success.
After a second round, Jenny and Lewis were told she was pregnant on January 14 - three days before her 35th birthday.
“It was the best birthday present ever,” she said. “I was so shocked, I didn’t think it would work. It made me think it was quite ironic that it continued the story that began 37 years ago. Felix is worth every penny and more.”
The couple went to on of the 14 CARE clinics and satellite clinics in the UK headed by Dr Simon Fishel, who was a PhD student with Dr Edwards at Cambridge in the Seventies, and is now the clinics’ chief executive and president.
He had worked with Dr John Webster, the former Oldham and District Hospital senior registrar, now a retired Fellow of the Royal College of Obstetricians and Gynaecologists, and who both helped set up Bourn Hall with Mr Steptoe and Dr Edwards in 1980, Dr Webster as deputy medical director, and Dr Fishel as deputy scientific director.
Dr Webster, who was Mr Steptoe’s right-hand man and assisted at the birth of Louise Brown, believes it was not the IVF breakthrough that was Mr Steptoe’s greatest achievement, but his pioneering work in laparoscopy or “keyhole” surgery, which was his most valuable skill.
Dr Webster said: “Laparoscopy has to be the bigger miracle, medically, than IVF, though you can’t tell that to someone who is infertile. In the 1960s, Patrick Steptoe was the laparoscopy pioneer.”
That skill brought Steptoe and Edwards together. The Cambridge scientist, later a professor and Nobel Prizewinner for medicine in 2010, had found a way of fertilising human eggs: in Steptoe he found someone who could develop the minimally-invasive technique using small incisions in a woman’s abdomen, to insert fine tubes and cold white light to “see” inside the body to collect eggs.
The technique avoided the risks of conventional surgery and drastically shortened recovery time.
Mr Steptoe, with Robert Edwards, helped to perfect a remarkable technique and since Louise, over five million women around the world, including my daughter, have good reason to say thank-you to him.
Most Viewed News Stories
- 1Milan Bar in Lees and The Bank at Delph close doors with immediate effect
- 2Latics announce retained list
- 3Punch perfect Kyle is Oldham's latest national boxing champ
- 4Second-hand music, books and media shop opens in Mossley
- 5Attack on shop worker filmed and posted on Snapchat results in jail sentence for Oldham man